In-Home Foot-Forward Care
Belle brings gentle, preventive care right to your home helping you stay comfortable, independent, and moving with confidence as we support your full body health.
See why 97% of our patients return for personalized, in-home foot-forward care.
How Our Service Works
Our in-home visits are designed to be easy, fun and most importantly protect your health and independence. Here’s what a typical appointment may include:
-

Meet your Community Health Worker
Your friendly, Belle-Certified Community Health Worker will come to your home with everything needed and will be your support guide for every visit.
-

Health Assessment
We’ll get to know you, your health and goals, and check your feet, vitals and mobility to catch issues early.
-

Preventive Care That Feels Good
Your visit regularly includes foot screenings and preventive care clinically proven to manage chronic conditions. Care includes light exfoliation, nail care and a soothing massage to boost circulation and skin health.
-

Enhanced Care Support
Every Belle-Certified Community Health Worker is backed by an integrated care team who reviews every visit. A Belle clinician will step in if more support is needed.
-

See You Next Month
Most members are eligible for monthly visits, but you set the pace. We’re here when you’re ready.

Always Here for You
Your integrated care team is available 24/7 to check in, answer questions, and support your journey to better health.
Backed by Results, Trusted by Thousands
Belle’s in-home care isn’t just convenient and comforting – it helps you stay healthier, happier and more independent right where you are.
In studies with health plans involving over 350,000 people, we’ve observed regular Belle visits lead to life-changing results:
- 58% reduction in open wounds
- 52% reduction in falls
- 48% reduction in nursing home needs
- 40% reduction in major depression
- 14% reduction in ER or hospital visits
These aren’t just numbers — they mean more good days, more confidence, and more peace of mind for you and your loved ones.
Offered Through These Health Plans
Belle is proud to work with trusted health plans so our services are often at little to no cost to you.





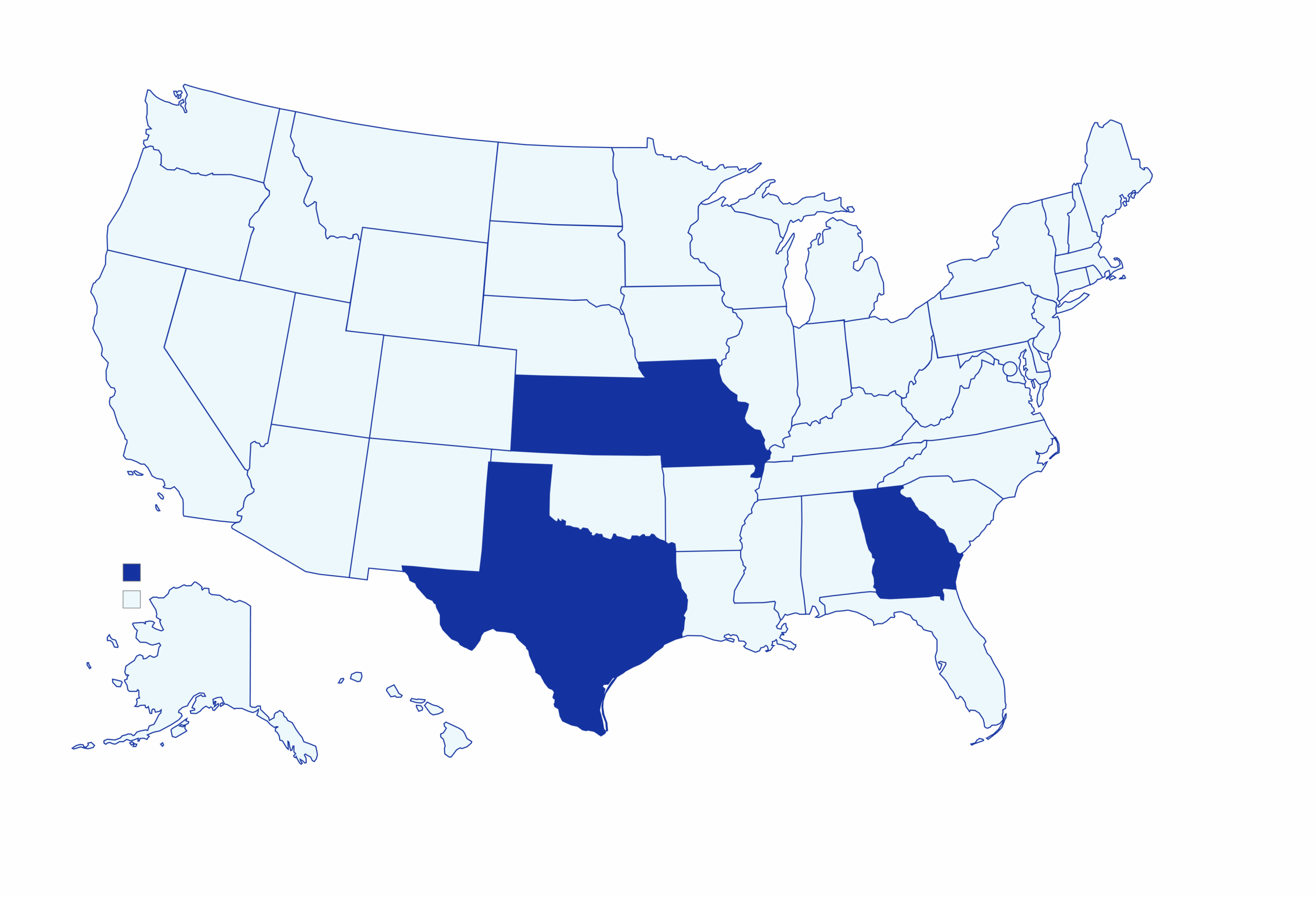
Where We Serve
We serve eligible members across Georgia, Texas, Missouri and Kansas. Give us a call at 855-232-7888 to see if we can serve you!

Belle helped me feel more in control of my health. I felt seen, heard, and truly cared for
I wasn't feeling myself due to medical issues, but when you walked in, it was like sunshine. You uplifted me with your smile and the small conversation we had while you took care of me.
It felt like catching up with an old friend—and my feet have never felt better!